
How Neighborhoods Affect the Health and Well-Being of Older Americans
Neighborhood characteristics affect people of all ages, but older adults—classified here as adults over age 50—may be affected more than other groups.
Older people typically experience higher levels of exposure to neighborhood conditions, often having spent decades in their communities. They have more physical and mental health vulnerabilities compared with younger adults, and are more likely to rely on community resources as a source of social support. As older adults become less mobile, their effective neighborhoods may shrink over time to include only the immediate areas near their homes (Glass and Balfour 2003).
This report summarizes recent research conducted by National Institute on Aging-supported researchers and others who have studied the association between neighborhood characteristics and the health and well-being of older adults. This research can inform policy decisions about community resource allocation and development planning. A growing body of research shows that living in disadvantaged neighborhoods—characterized by high poverty—is associated with weak social ties, problems accessing health care and other services, reduced physical activity, health problems, mobility limitations, and high stress.
This area of research is challenging because lower-income people tend to live in disadvantaged neighborhoods and many detrimental neighborhood features cluster together. Disadvantaged neighborhoods often have more crime, more pollution, poorer infrastructure, and fewer health care resources—making it difficult to pinpoint which neighborhood feature is responsible for particular health outcomes.
Some researchers continue to focus on a single neighborhood feature and may incorrectly attribute health effects to the wrong characteristics. Others have created scales consisting of multiple features that are found together, which can mask the features that matter the most. In addition, most results are based on cross-sectional data (subjects interviewed at one point in time only) and may reflect people with more resources and in better health moving out of disadvantaged neighborhoods and those with fewer resources and worse health moving in or staying (Grafova et al. 2014). While existing research is not yet able to pinpoint exactly how neighborhoods cause changes in physical and cognitive health, researchers have identified a number of strong associations that point to possible pathways.
Neighborhood Disadvantage and Health
Neighborhood economic status—often measured by median household income or the share living below the poverty line—is one of the most widely studied and strongest predictors of the health and well-being of older adults. Older residents of economically disadvantaged neighborhoods are more likely to have chronic health and mobility issues and die at younger ages compared with older residents in more affluent communities. In part, these differences can be explained by the characteristics of people living in these neighborhoods, but a growing number of studies also suggest that neighborhood characteristics may independently influence older residents’ health and well-being.
Freedman, Grafova, and Rogowski (2011) use data from the Health and Retirement Study (HRS), which follows a nationally representative group of older adults, to look at the effects of neighborhood characteristics on six common chronic diseases: hypertension, heart problems, stroke, diabetes, cancer, and arthritis. They find that women living in disadvantaged neighborhoods are more likely to develop heart disease, even after controlling for individual characteristics and aspects of the physical environment (such as population density, pollution, and walkability). In another study using HRS data, Grafova and colleagues (2008) find that adults ages 55 and older living in more affluent neighborhoods are less likely to be obese, after accounting for individual differences and family characteristics.
Neighborhood conditions can also influence older adults’ self-perceived health status. Using data from the Study of Asset and Health Dynamics Among the Oldest Old (AHEAD), Wight and colleagues (2008) find that adults ages 70 and older living in economically disadvantaged neighborhoods are more likely than their peers living in wealthier neighborhoods to report being in poor health. In fact, living in a disadvantaged neighborhood has a greater negative association with self-rated health status than either cardiovascular disease or functional limitations. Self-rated health is important because it reflects a person’s overall appraisal of their physical and/or mental health and tends to be closely related to a person’s actual health status.
Compared with cross-sectional studies that interview subjects at only one point in time, studies that capture neighborhood socioeconomic conditions earlier in life and track individuals over many years provide stronger evidence of whether living in a disadvantaged neighborhood is associated with poorer health later in life. Estimates based on the Panel Study of Income Dynamics show that living in low-income neighborhoods during young adulthood is strongly associated with poor health in later life (Johnson, Schoeni, and Rogowski 2012). The researchers find that one-quarter of the variation in mid-to-late-life health is linked to neighborhood disadvantage after accounting for individual and family differences. In another study, Glymour and colleagues (2010) measure neighborhood disadvantage with a six-indicator index, using HRS data that tracked respondents ages 55 to 65 over 18 years. Focusing on respondents who were disease free before the study began and statistically accounting for neighborhood change, they find that living in a disadvantaged neighborhood is associated with a greater likelihood of reporting poor self-rated health, but not disability or elevated depressive symptoms.
The level of income inequality in a local area may also influence health. Using HRS data, Choi and colleagues (2015) compare health outcomes of adults ages 50 and older with similar socioeconomic profiles in high-inequality and low-inequality U.S. counties. They find that older adults in counties with high levels of inequality report worse health status and more psychiatric problems than older people in low-inequality counties. Although the authors do not establish a causal link between income inequality and health status, they argue that high levels of inequality may contribute to “systematic underinvestment” in communities that could leave residents with “fewer resources to buy housing, healthy food, and medical care.” Income inequality may also be associated with lower levels of social cohesion and trust, leading to stress that affects residents’ mental and physical health, they suggest.
Effects on Mortality
Extensive research has examined the link between neighborhood characteristics and mortality, but few studies have focused on this relationship among older adults. Using data from the Americans’ Changing Lives (ACL) survey, Yao and Robert (2008) find no significant association between living in a disadvantaged neighborhood and the mortality of adults ages 60 and older, after accounting for individual socioeconomic and health characteristics.
Wight and colleagues (2010) take this line of research a step further by examining the potential impact of multiple neighborhood characteristics on the risk of death among urban adults ages 70 and older, using data from the AHEAD study. Similar to Yao and Robert, they find no link between living in a disadvantaged neighborhood and risk of mortality after accounting for individual characteristics. People living in neighborhoods with a high proportion of Hispanic residents were at increased risk of mortality—a finding contrary to expectations that immigrant enclaves protect health by providing a source of social support for older adults. Ultimately, however, this risk was not significant after accounting for neighborhood affluence. Residents of affluent urban areas may be more aware of cutting-edge health care innovations and more likely to have the financial means to take advantage of them, the researchers suggest.
Effects on Disability
Neighborhood conditions can also affect the likelihood of older adults having functional limitations, such as difficulty walking. Freedman and colleagues (2008) look at the relationship between neighborhood conditions and disability among adults ages 55 years and older using HRS data. They find that older adults living in economically advantaged communities are less likely to develop problems with lower-body functioning compared with older adults in economically disadvantaged areas. Living in more affluent communities may help stave off functional problems during the early stages of disability, while living in disadvantaged communities may exacerbate functional limitations during the latter stages of decline. The authors argue that older people with greater wealth may be better able to prevent disease and disability, while those with limited income may be less able to fully recuperate or to adapt their homes to accommodate their functional decline.
Most researchers have focused on the effects of current neighborhood characteristics on health. But results based on this type of point-in-time approach may underestimate the effects of neighborhood characteristics on individuals over the life course. Clarke and colleagues (2014) use data from the ACL study to investigate the cumulative effects of neighborhood characteristics on functional decline among adults ages 25 and older over a 15-year period. They find that, over time, living in disadvantaged neighborhoods contributes to a 20 percent increase in the odds of developing a functional limitation and a 40 percent increase in the odds of dying, after controlling for racial/ethnic composition and individual socioeconomic factors. Although the study focuses on adults of all ages, older adults may face higher risks because they are more likely to live in disadvantaged neighborhoods and are much more likely than younger adults to die or experience functional limitations over time.
Cumulative Disadvantage and “Weathering”
Long-term exposure to stress in disadvantaged neighborhoods may lead to “weathering,” a “cumulative biological impact of being chronically exposed to, and having to cope with, socially structured stressors,” explain Geronimus and colleagues (2015). The researchers argue that weathering can “increase health vulnerability and accelerate aging in marginalized populations.” For example, Geronimus and colleagues examine telomere length—an aspect of chromosomes that shortens with stress and aging—in a small sample of older residents from three Detroit neighborhoods. They link high levels of self-reported stress regarding personal safety to shorter telomeres and high levels of neighborhood satisfaction to longer telomeres.
King, Morenoff, and House (2011) find that neighborhood affluence is associated with fewer biological risk factors for chronic disease (such as high blood pressure and elevated cholesterol levels) after adjusting for individual-level social and economic background, using data from the Chicago Community Adult Health Study (CCAHS) on adults of all ages. Also using the CCAHS, King (2013) links neighborhood walkability to lower concentrations of C-reactive protein (CRP) in adults of all ages—a protein linked to inflammation, infection, and developing tissue damage and heart disease. But the same study links neighborhood density (a neighborhood feature sometimes related to walkability) to an increase in CRP, suggesting that aspects of densely populated neighborhoods—such as sleep-disturbing noise and pollution—may take a toll on health over time.
Effects on Cognitive Decline
Clarke and colleagues (2012) show that living in an affluent community has a positive impact on the cognitive function of residents, after accounting for individual background, health, and risk factors. For the study, they use data from the Chicago Health and Aging Project (CHAP), which surveyed a racially diverse group of more than 6,000 adults ages 65 and older over 18 years in three adjacent Chicago neighborhoods. Using AHEAD data, Wight and colleagues (2006) show that adults ages 70 and older living in neighborhoods with low overall education have lower cognitive function than older adults living in areas with high education levels, independent of the elderly individuals’ own education and income level.
Aneshensel and colleagues (2011) find similar results when they link HRS responses with census data on neighborhood characteristics. Their findings show that living among more advantaged neighbors is associated with higher levels of cognitive function among people ages 55 to 65 with low education and income levels. Conversely, they find that older people with low socioeconomic status living in impoverished neighborhoods face the highest risk of poor cognitive function. They conclude that “being poor in a poor neighborhood” compounds the disadvantage. The researchers recommend neighborhood-level interventions that reduce disparities, such as “safe and accessible community centers where residents of poor neighborhoods can meet to discuss shared problems, obtain information about community activities, and interact with people with a wide range of life experiences.”
Neighborhood Walkability and the Physical Environment
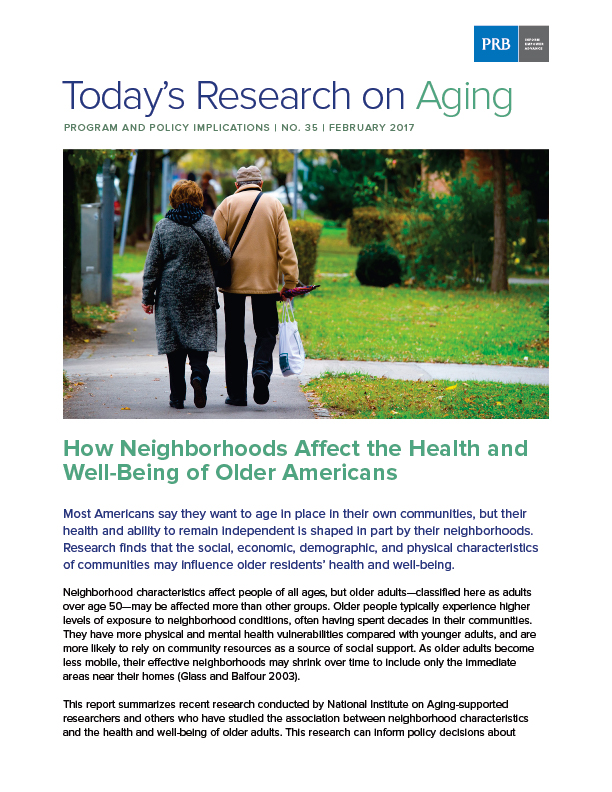
It is not only the economic characteristics of neighborhoods that affect health—but also aspects of the physical or “built” environment that promote walkability and foster interaction (see Table). Certain neighborhoods that are less accessible are particularly challenging for older adults with disabilities.
Tomey and colleagues (2013) find that neighborhood levels of sociability and walkability are positively linked to self-rated health among adults ages 45 to 84 in the Multi-Ethnic Study of Atherosclerosis (MESA). Neighborhood walkability, as measured through street connectivity—a higher number of intersections and fewer dead-end streets or cul-de-sacs—has also been linked to a lower risk of self-reported disabilities and lower obesity rates (Freedman et al. 2008; Grafova et al. 2008).
The condition of neighborhood streets and sidewalks can make a big difference in the mobility of adults who have difficulty walking, according to Clarke and colleagues (2008). Adults with severe impairments are four times more likely to report a mobility disability if they live in neighborhoods with numerous cracks, potholes, or broken curbs in streets and sidewalks, according to their analysis of the cross-sectional CCAHS. The researchers suggest that if street quality could be improved, adults at greatest risk for disability could remain mobile and function independently for a longer period of time.
In a subsequent analysis using data from the ACL study, Clarke, Ailshire, and Lantz (2009) find that adults ages 75 and older living in compact neighborhoods with more accommodations for pedestrians are less likely, over a 15-year period, to report a mobility disability compared with those living in neighborhoods that are less pedestrian-friendly.
Among older adults with disabilities, well-designed neighborhoods can enhance outdoor activity. Older adults may be more likely to walk outside in pedestrian-friendly neighborhoods that they perceive as safe. For example, Satariano and colleagues (2010) find that older adults living in less compact residential areas—such as sprawling suburban neighborhoods—spend less time walking per week compared with those living in mixed-use or commercial areas. The authors argue that more compact communities may provide more walking destinations for older adults. However, compact neighborhoods are not associated with walking among those with poor functional capacity, who may perceive these areas as being less safe. “A compact area may have more walking destinations, but it also may have more streets to cross, cars to avoid, and greater pedestrian density,” the researchers note.
Similarly, Clarke and Gallagher (2013) find that older adults living in more accessible neighborhoods are more likely to walk outside in a typical week compared with those in less-accessible neighborhoods. Their study investigates the relationship between the built environment and mobility disability among adults ages 55 and older in Michigan. They create an innovative “accessibility score” using Google Earth’s “Street View” to measure pedestrian-friendly features such as smooth, barrier-free sidewalks and access to public transportation on the street.
Additionally, a study by Gallagher, Clarke, and Gretebeck (2014) shows that poor sidewalk design and perception of crime are associated with shorter walks. Women take longer walks if they have a destination, such as a friend’s house, while men are more likely to walk longer distances in higher-density, pedestrian-friendly communities.
Neighborhood Physical Environment and Cognitive Function
The stress of living in disorderly neighborhoods (measured by the presence of trash, vandalism, safety problems, and broken curbs and sidewalks) appears to take a toll on the cognitive functioning of residents, according to Boardman and colleagues (2012). They focus on the gene APOE-E4 that has been linked to early-onset cognitive decline and is more common in people diagnosed with Alzheimer’s disease. Using CHAP data, they showed that older adults who carry the APOE-E4 gene have lower levels of cognitive function that decline more rapidly over time than those without the gene. But they demonstrate that the gene has the largest impact on the cognitive function of carriers who live in the most orderly neighborhoods, suggesting that when negative social conditions are eliminated, the genetic influence on cognitive function becomes more apparent.
Neighborhoods with more resources—parks, recreation centers, community centers, libraries—may buffer residents’ cognitive decline by creating greater opportunities for social interaction and physical activity. After taking into account individual background and health conditions, Clarke and colleagues (2015) use CHAP data to show that older people living in neighborhoods with community centers, accessible public transit, and well-maintained public spaces such as sidewalks tend to experience slower cognitive decline than similar adults whose neighborhoods lack these features. The researchers underscore the importance of keeping public spaces in good condition and maintaining barrier-free walkways, which may “support physical, social, and leisure activities for older adults.”
Recent studies demonstrate a link between exposure to higher concentrations of fine particulate matter air pollution and lower levels of cognitive function in older adults, even after taking economic and social differences into account. Inhaling small particles can damage organs, including the brain. Ailshire and Clarke (2015) examined a sample of non-Hispanic black and white men and women ages 55 and older from the 2001/2002 ACL study. They paired individuals’ tests of working memory and orientation with census tract level Environmental Protection Agency air monitoring data. Those living in areas with high concentrations of fine particulate matter pollution made 50 percent more errors than those exposed to lower air pollution levels. “Air pollution may represent an important modifiable risk factor for poor cognitive function in older adults,” the researchers assert. In a similar study using HRS data, Ailshire and Crimmins (2014) also find a link between fine particulate matter air pollution and cognition, particularly episodic memory. “Improving air quality in large metropolitan areas, where much of the aging U.S. population resides, may be an important mechanism for reducing age-related cognitive decline,” they suggest.
Neighborhood Food Environment and Health
Neighborhood characteristics can also affect health by influencing the food residents eat. Kaiser and colleagues (2016) find that MESA participants who live in neighborhoods with healthier food environments—greater access to fruits and vegetables and to low fat foods—have a lower risk of developing high blood pressure. These findings suggest that “healthy food environments are associated with better diets and that better diets can reduce hypertension risk.”
While living in healthier food environments contributes to better health outcomes, living in unhealthy environments is associated with increased health risks. For example, Morgenstern and colleagues (2009) document that living in a neighborhood with a higher density of fast food restaurants is associated with an increased risk of ischemic stroke among participants in the Brain Attack Surveillance in Corpus Christi (BASIC) project.
Neighborhood Safety and the Social Environment
Older residents’ sense of neighborhood safety is key to their physical activity levels, particularly among those with disabilities. Using HRS data, Latham and Clarke (2013) find that older adults in neighborhoods perceived as safe are more likely to recover from a mobility limitation. The social environment also plays a role in recovery: Older adults who socialize with their neighbors are most likely to partially or fully recover from a severe mobility limitation (Latham, Clarke, and Pavela 2015). Those least likely to recover include women who have no neighborhood friends. The researchers suggest that “interventions aimed at encouraging older adults with mobility limitations to be engaged in their neighborhood” may contribute to improved physical functioning. However, older adults living in the same neighborhood as relatives are less likely to recover from a mobility limitation. Relatives may help people remain in their homes, but “overdependence on assistance from nearby family members could arise and have negative consequences for functional health and recovery,” they write.
Neighborhood safety is related to physical activity levels of older people of all socioeconomic backgrounds, report Tucker-Seeley and colleagues (2009) based on HRS data. Older people who perceive their neighborhoods as safe are more likely to engage in outdoor physical activity than those who consider their neighborhoods unsafe. The researchers suggest that programs designed to promote physical activity among older people should consider neighborhood safety concerns as potential barriers to participation.
Strong neighborhood social networks may blunt the “widow effect”the well-established finding that the death of a spouse increases the surviving partner’s risk of death. Subramanian, Elwert, and Christakis (2008) find that widowed men and women living in neighborhoods with high concentrations of older adults who have lost a spouse are less likely to die than those in neighborhoods with low concentrations. They suggest that in neighborhoods where widowhood is more common, widows and widowers may be more able to find similar individuals and renew or establish friendships that help replace the social support and companionship lost at a partner’s death.
Ethnic Enclaves, Residential Segregation, and Older Adults’ Well-Being
Ethnic enclaves may protect the health of older adults in disadvantaged communities by supporting healthy behaviors and through stronger social networks. Data from the HRS show that residents of highly segregated Hispanic neighborhoods have higher levels of cognitive function (Kovalchik et al. 2015). But over time, individuals living in neighborhoods with high concentrations of Hispanics are more likely to experience rapid cognitive decline than people living in more integrated settings. The researchers suggest that strong social networks and multilingualism may create a “cognitive reserve” that raises the threshold at which cognitive deficits emerge. However, “once life stressors have accumulated and a clinical threshold for neurological damage has been passed, the decline in cognition is more precipitous,” they write.
While ethnic enclaves may be a source of social support for older adults, they can also signal high levels of racial/ethnic segregation, which can negatively affect health. A recent study links living in a neighborhood with high levels of segregation (concentrations of racial/ethnic minorities) combined with high crime to an elevated risk of cancer among older men and women (Freedman, Grafova, and Rogowski 2011). These neighborhood stressors may contribute to “a stress response that interrupts the body’s ability to fight cancer cell development,” according to the researchers.
Osypuk and colleagues (2009) study Hispanics living in neighborhoods with high concentrations of Latin American-born immigrants and find low levels of high-fat foods in their diets but also low levels of physical activity. Using HRS data, Grafova and colleagues (2008) also find that older men living in immigrant enclaves are more likely to be obese.
In another study using HRS data, Sudano and colleagues (2013) find that living in racially segregated neighborhoods (those with high shares of minorities) is linked to poor health largely because the older residents in these communities have less education, higher poverty rates, and lower levels of net worth compared with older adults in less segregated communities.
Kershaw and colleagues (2015) document that segregation affects cardiovascular risk differently for whites and for racial minorities. They find that living in highly segregated black neighborhoods is linked to a higher risk of cardiovascular disease (CVD) among black MESA participants followed over 10 years. Conversely, living in more segregated white neighborhoods is linked to a lowered risk of CVD among white MESA participants.
Conclusions
Research on the ways neighborhood settings affect health, like all epidemiological research, allows researchers to describe risk factors and associations but not to estimate direct cause and effect. Nevertheless, the strong patterns identified by this research can help policymakers and planners design new health-promoting policies and better target intervention programs. In some cases, improving neighborhood safety or making changes to the neighborhood’s built environment improving sidewalks, for example may be more cost-effective ways to improve health outcomes among older adults than changing individuals’ health behaviors.
The potential negative effects of living in disadvantaged neighborhoods for the physical and mental health of older adults point to the need for neighborhood improvements that expand the quantity, quality, and accessibility of community resources (such as parks, libraries, and community centers) and enhance walkability and safety. For others in more affluent communities, policies should help older adults age in place so that they can live independently longer, avoiding or postponing the need for costly long-term care.
Some of the results suggest that different interventions may be needed for men versus women. For example, women are more likely to take long walks—an excellent way to maintain physical fitness—if they have a particular destination, while men are more likely to take walks in pedestrian-friendly communities. Older adults living with disability also have different needs than those without limitations, especially among those who may be isolated in less accessible or unsafe communities.
Future research should consider the longer-term impact of neighborhood characteristics over an individual’s lifespan. Although an individual’s neighborhood setting is recognized as having a cumulative effect, few studies take a longitudinal approach, often due to limitations in the available data. Given the persistent racial/ethnic disparities and high levels of racial/ethnic segregation in many U.S. neighborhoods, more research is needed to investigate the role of segregation on health outcomes among older adults and how to address it.
References
Jennifer Ailshire and Philippa Clarke, “Fine Particulate Matter Air Pollution and Cognitive Function Among U.S. Older Adults,” Journals of Gerontology, Series B: Psychological and Social Sciences 70, no. 2 (2015): 322-8.
Jennifer Ailshire and Eileen Crimmins, “Fine Particulate Matter Air Pollution and Cognitive Function Among Older U.S. Adults,” American Journal of Epidemiology 180, no. 4 (2014): 359-66.
Carol Aneshensel et al., “Are Neighborhood Socioeconomic Disadvantage and Racial/Ethnic Segregation Associated With Cognitive Functioning in Late Middle Age?” Journal of Health and Social Behavior 52, no. 2 (2011): 162.
Jason Boardman et al., “Social Disorder, APOE-E4 Genotype, and Change in Cognitive Function Among Older Adults Living in Chicago,” Social Science & Medicine 74, no. 10 (2012): 1584-90.
HwaJung Choi et al., “Are Older Adults Living in More Equal Counties Healthier Than Older Adults Living in More Unequal Counties? A Propensity Score Matching Approach,” Social Science & Medicine 141 (2015): 82-90.
Philippa Clarke, Jennifer Ailshire, and Paula Lantz, “Urban Built Environments and Trajectories of Mobility Disability: Findings From a National Sample of Community-Dwelling American Adults (1986-2001),” Social Science & Medicine 69, no. 6 (2009): 964-70.
Philippa Clarke and Nancy Ambrose Gallagher, “Optimizing Mobility in Later Life: The Role of the Urban Built Environment for Older Adults Aging in Place,” Journal of Urban Health 90, no. 6 (2013): 997-1009.
Philippa Clarke et al., “Cognitive Decline and the Neighborhood Environment,” Annals of Epidemiology 25, no. 11 (2015): 849-54.
Philippa Clarke et al., “Cognitive Function in the Community Setting: The Neighbourhood as a Source of ‘Cognitive Reserve’?” Journal of Epidemiology and Community Health 66, no. 8 (2012): 730-6.
Philippa Clarke et al., “Cumulative Exposure to Neighborhood Context: Consequences for Health Transitions Over the Adult Life Course,” Research on Aging 36, no. 1 (2014): 115-42.
Philippa Clarke et al., &ldqu

 ">
">
